WHY MEASURE TEMPERATURE TO SCREEN FOR INFLUENZA VIRUSES SUCH AS COVID-19 (SARS-COV-02)
The key reason for measuring temperature is that we can detect individuals with a fever – and a fever is the EARLIEST and MOST COMMON symptom of all influenza infections.
So we should consider what is normal body temperature and what is a fever?
For healthy individuals a body temperature – measured orally – of between 97 °F (36.1 °C) and 100 °F (37.8 °C) is considered normal (the average being 98.6 °F (37 °C)). Note that a “normal” temperature range is different for each individual person, and an individuals temperature varies during the day, normally higher in the afternoon.
A fever simply describes a temperature that is higher than the body’s normal healthy working range and is a temperature above that which the body’s heat management system can regulate.
The reason that the human body increases its temperature in response to an infection is that an elevated body temperature is an important component of the body’s immune response. Higher temperatures increase the production of cells that fight off the invading bacteria or viruses, inhibit the growth of some bacteria, while at the same time speeding up the chemical reactions that help the body’s cells repair themselves, and finally speeds the arrival of white blood cells to the sites of infection.
Irrespective of individual temperature variability medically it is considered that a fever exists when the body temperature is at, or above, 38 deg C (measured orally), although many nursing professionals use a temperature of above 37.8 deg C as indicating the body is fighting an infection in most people.
Note that skin surface temperature of the head (which our infra-red thermographic cameras measure) is 0.3 – 0.6 deg C lower the orally measured temperature. From experience we have found that setting the fever alert threshold temperature at between 37.2 deg C and 37.4 deg C – depending on the environment – achieves the best results with our cameras.
WHY EVERYONE SHOULD BE CONCERNED ABOUT HAVING THE CAPABILITY TO QUICKLY IDENTIFY INFLUENZA INFECTIONS
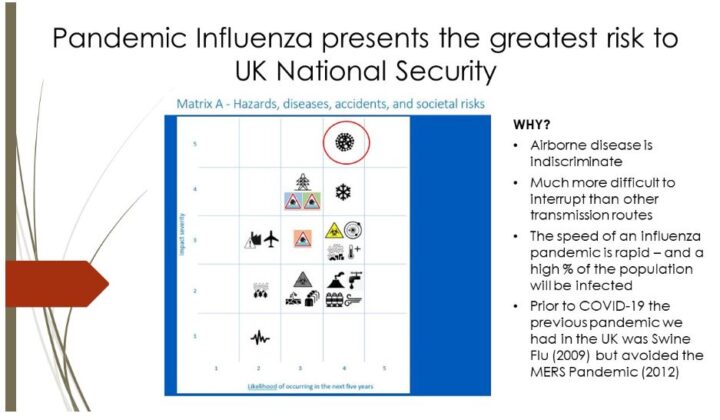
- Pandemic Influenza represents the greatest risk to UK National Security*. “Pandemic Influenza by far remains, by a very very long distance, our biggest known epidemic risk”, Prof. Chris Whitty (Chief Medical Officer for England)) Gresham College Lecture October, 2018.
- Should a new influenza outbreak occur it will take months before large scale sample testing becomes available. In this initial period one of the only means of screening for individuals that could be infected is through using temperature measurement.
- In the case of COVID-19 the virus (SARS-COV-02) is highly contagious and in retrospect we now know that every day’s delay there was in implementing prevention measures allowed a significant increase in the number of people being infected.
- Insufficient preparedness has been the main reason that the UK has not managed the COVID-19 epidemic as well as many South East Asian Nations that – after the MERS Epidemic of 2012 – had put in place measures to be better prepared for the next influenza epidemic. Temperature Testing being an important part of this program.
Bangkok,Thailand – April 07 2020. Temperature control zone, Siam paragon shopping mall in Bangkok during Coronavirus, COVID-19 outbreak.
- It is not just a new epidemic or pandemic influenza that we need to be worried about. Seasonal influenza (The “Flu”) kills 20,000** individuals every year in the UK and temperature monitoring can be used to screen for individuals infected with the “Flu” virus just as affectively as COVID-19…. or for that matter any new Influenza virus.
- Even after effective vaccines for COVID-19 are developed and are available on a mass scale (assuming one will be developed***) it will not eliminate the SARS-COV-02 virus and its derivatives and it will not prevent on-going illness and deaths. We obviously do not know the legacy affect of COVID-19 but vaccines for the seasonal flu have existed since the 1930’s and this still kills 20,000 people in the UK every year.
- There is also a high probability that another pandemic influenza outbreak will hit the UK within the next few years and the wide spread use of temperature screening can help prevent a repeat of the severity of the COVID-19 outbreak.
* National Risk Register Of Civil Emergencies 2017, Cabinet Office 70 Whitehall London SW1A 2AS © Crown copyright 2017, Published September 2017.
**Average number of annual UK deaths between 2016 and 2019 (7.6 Million Working days lost annually to the seasonal flu – Research by the Co-operative Group in 2010)
*** Coronaviruses were first discovered in the mid 1960s and there are currently 7 identified coronavirus that infect humans (229E, NL63, OC43, HKU1, MERS-COV, SARS-COV and SARS-COV-2 (the virus that causes COVID-19)). TO DATE THERE HAS BEEN NO SUCCESSFULL VACCINE DEVELOPED FOR ANY CORONAVIRUS.
WHY USE INFRA-RED THERMOGRAPHY TO DETECT A FEVER?
- Infra-red thermography is currently the only viable means of mass screening people who are likely to be carrying an influenza virus****.
- The effectiveness of the temperature measurement is similar to that of the currently available rapid sample test kits, however with temperature measurement the results are instant and there is not limit – or cost – to how many tests are performed.
- Provides a non-contact and safe socially distanced temperature measurement test process.
- Staff are not required to take physical samples and there are no additional costs of managing tests and handling samples.
- After the initial outlay there is nominal running costs and no risk of running out of testing capability (As we write this 6 months after COVID-19 was officially recognised as a pandemic there is currently a shortage of testing capability in the UK)
- Human skin is an almost perfect emitter of infrared energy. When you consider that the body uses the skin to transfer 80% of its heat energy away from the body, and there has been 6 million years of evolution to perfect this, it probably should not be so surprising that the skin is this efficient!
- Skin pigment has negligible influence on accuracy of thermal cameras so the measurement is valid for all ethnicities.
- The face provides an ideal “target” for infra-red thermographic cameras and the Vision camera systems can also measure accurate temperature when face masks and glasses are worn.
**** At the time of writing it is 6 months after COVID-19 was officially recognised as a pandemic, and 9 months after the genome sequence was identified (which enabled the pharmaceutical companies to start making test kits) the alternatives to temperature measurement – which are all sample collection based tests – are not practical for mass screening and in most cases are less effective than temperature measurement in the early stage identification of a virus. For more information on the alternative tests please follow this link.
WHAT ACCURACY SHOULD YOU EXPECT FROM THERMOGRAPHIC CAMERAS
- Perhaps the most important factor to understand before deploying thermal cameras is that they are not a go – no go test they simply detect one symptom – the most common symptom – of an influenza infection. Real world research is hard to find but the information that is available points to a real world detection rate of between 30% and 50% of people who are infected when the infection rate is stable. This is comparable with the accuracy of the current rapid COVID-19 sample tests
- A study into the estimated effectiveness of screening travellers for potential COVID-19 infection (Using both fever measurement and self-reporting questionnaire/ interview screening measures) estimate that between 25% and 60% of individuals that are carrying the COVID-19 virus will be detected when the epidemic is stable *****.
- A recent paper in the New England Journal of Medicine shows that most people are infected with the new coronavirus for just over five days before showing symptoms. Using this information, combined with data on the sensitivity of thermal scanners, the LSHTM****** team used a mathematical model to estimate that for every 100 infected travellers planning to take a 12 hour flight, 9 will be detected at entry screening upon arrival and 49 passengers would be detected through exit screening before they board, but 42 infected travellers will pass both exit and entry screening undetected. The precise numbers depend on how good screening is at detecting symptoms as well as the time periods between infection and illness.
- The US Food and Drug Administration (FDA) state that “Some studies suggest that temperature measurements alone may miss more than half of infected people*******”.
- In many of the environments that thermal cameras can be deployed individuals will be screened at the very least daily, and in many scenarios multiple times each day. We have not yet seen any specific research into the effectiveness of temperature screening in a normal office, factory, shopping or educational environment. However, we would expect the detection rate to be higher than at transport hubs (which the studies seem to have mainly focused on) where there is mainly a transient movement of people and increased likelihood of people trying to cover up symptoms.
- For more information on the most common factors that can reduce the accuracy of temperature screening please follow this link.
***** Gostic, K.M. Gomez, A.C.R., Mummah, R.O., Kucharski, A.J., Lloyd-Smith J.O., Estimated effectiveness of symptom and risk screening to prevent the spread of COVID-19. eLife, 2020. 9 e55570
****** London School of Hygiene and Tropical Medicine , How effective is thermal scanning at airports?. 30 January 2020
******* FDA., “Non-contact Temperature Assessment Devices During the COVID-19 Pandemic“, 19-06-2020
THE VISION ADVANTAGE
- The Vision infra-red thermographic cameras combine face or body recognition technology with high accuracy infra-red temperature measurement sensors.
- Vision systems do not require a POS (Point of Screening) station to be staffed and the results can be discretely monitored by a reception desk, security office or remote office.
- Inaccuracies using hand held devices due to improper use, accuracy of the device or improper maintenance are avoided.
- Because the Vision camera systems are fully automatic they do not rely on a human tester – Human testing often becomes more casual and less diligently performed over time.
- The risk of transfer of the virus by sharing a hand-held measuring device is eliminated.
- The risk of transfer of virus by close proximity with a virus carrier is eliminated.
- Incorrect or incomplete identification of individuals with a fever can be prevented and avoids potential transfer of infection caused by the sharing of writing equipment, computer or tablet device.
- Images can be recorded of all individuals being tested helping improve contact tracing*******.
- All our systems can be remotely managed to ensure compliance that the systems are working correctly and being used correctly. Customers can manage their own devices or Vision can manage the systems on their behalf.
- The ongoing operational costs after the initial investment are negligible. The cheapest cost for a COVID-19 test that we have seen suggested could be achievable is £5.00 per test (cost are much higher that this at the moment). In addition the cost of staff, PPE and managing test samples is also avoided. Within 250 tests the THC-01 will have paid for itself compared to sample testing, and 3,000 tests the THC-02 will have paid for itself. Both of these cameras could pay for themselves within 1 hour compared to taking the same number of samples (although sample testing could not achieve anywhere near this throughput of people).
******** There should not be any conflict with GDPR requirements as these cameras provide “legitimate” and ” vital” reasons for recording images, but this feature can be turned off if required. Where CCTV is currently in use thermographic cameras should anyway be covered by existing GDPR policies.
OUR PRODUCTS
Vision offer two products to meet different environmental requirements
VIS-THC-01 BODY TEMPERATURE MEASURING SMART CAMERA
This Camera is best suited to screening up to 9 individuals per minute in a controlled environment. It is ideal for screening individuals entering a hospital ward, staff room, restaurants, shops or office.
Please follow this link for more information on the VIS-THC-01
The VIS-THC-02 Mass Temperature Measuring Smart Camera
This camera is best suited for high foot fall environments and can screen up to 10 individuals simultaneously and can screen 60+ people a minute, certainly capable of measuring a faster throughput than individuals walking past the camera with proper social distancing could reach.
With this camera it is very difficult for any individual to avoid being accurately measured – they would have to deliberately cover their face to avoid an accurate temperature reading
This camera is ideal for screening individuals in high foot fall uncontrolled environments. For example, entrances to public buildings, hospitals, libraries, schools, office blocks, department stores, large supermarkets, and factories with large workforces. The camera – or additional cameras – can be placed in corridors or and any area of high traffic density.
Please follow this link for more information on the VIS-THC-02